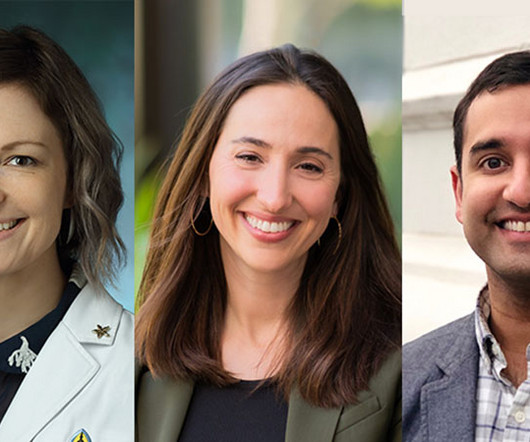
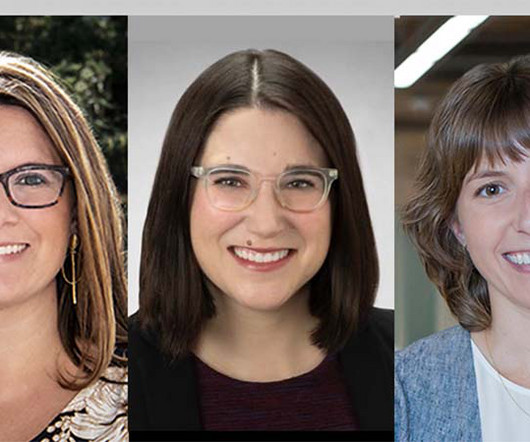
Honoring the Integral Role of Skilled Nurses
Traditions Health
MAY 11, 2025
Skilled nurses are vital to health care: They provide specialized care in a wide range of settings, including patients homes, care that requires advanced skills beyond basic nursing training. For these reasons and many more, National Skilled Nursing Care Week has been a national observance since 1967.










































Let's personalize your content