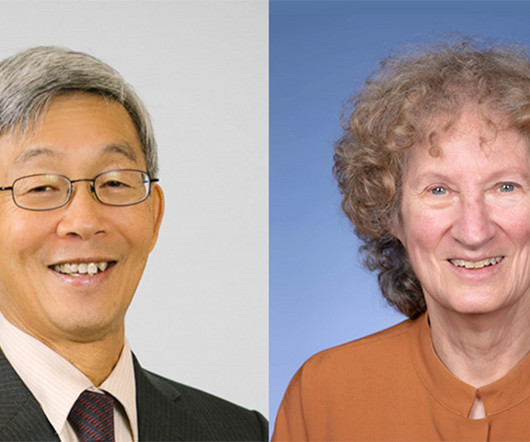
RCT of PC in ED: Corita Grudzen, Fernanda Bellolio, & Tammie Quest
GeriPal
APRIL 10, 2025
Summary Transcript CME Summary Early in my research career, I was fascinated by the (then) frontier area of palliative care in the emergency department. I asked emergency medicine clinicians what they thought when a patient who is seriously ill and DNR comes to the ED, and some responded, (paraphrasing), what are they doing here? They got feedback.













Let's personalize your content