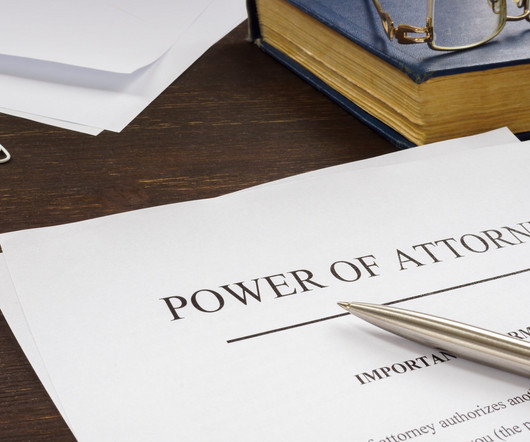
The Importance of an Advance Healthcare Directive
American In-Home Care
MARCH 15, 2024
Yet, one aspect of life often gets overlooked or pushed aside: planning for our healthcare needs, especially as we age. However, having an advance healthcare directive in place is not just for the elderly or those with serious medical conditions—it's important for everyone.





































Let's personalize your content